| Sol-Anhelo Pharmacy – Premium Healthcare Solutions Online | Home | Support | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Categories Home Diabetes |
:: PRICE LIST ::
Select Dosage:
[0,5mg]
[1mg]
[2mg]
:: PRODUCT INFORMATION ::
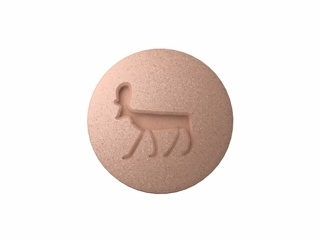
Mastering Post-Meal Glucose Spikes: Why Prandin is Your Key to Stable Blood SugarProblem Description: The Challenge of Postprandial HyperglycemiaDiabetes Mellitus, a chronic condition affecting millions globally, presents a significant daily challenge, particularly concerning the management of blood glucose levels after meals. This phenomenon, known as postprandial hyperglycemia, occurs when the body either does not produce enough insulin or cannot effectively use the insulin it produces to handle the influx of glucose absorbed from food. If left unchecked, these sharp spikes in blood sugar can contribute significantly to long-term complications associated with diabetes, including cardiovascular disease, neuropathy, and retinopathy. Many individuals find that while their fasting blood sugar levels might be somewhat controlled through lifestyle modifications or foundational medications, the peaks immediately following breakfast, lunch, or dinner remain stubbornly high. This inconsistent control can lead to fatigue, increased risk of hypoglycemia if overcompensated later, and overall poorer long-term health outcomes. Finding a medication that specifically targets this immediate post-meal surge is crucial for achieving comprehensive glycemic control. We must look beyond general glucose-lowering agents to find targeted solutions like Prandin. If you are frequently searching for "best medication for high blood sugar after eating", it is time to explore targeted therapies. Traditional oral agents often work by reducing hepatic glucose production or improving overall insulin sensitivity throughout the day. While effective for baseline control, they may lack the swift action required to manage the acute rise in blood sugar after carbohydrate consumption. For instance, while treatments like Metformin (a cornerstone therapy often mentioned alongside Metformin) are excellent for long-term management, they do not possess the rapid onset required for immediate post-meal regulation. This gap in treatment efficacy leaves a window open for damaging glucose excursions. Understanding the pharmacokinetics of rapid-acting insulin secretagogues is essential for patients seeking tighter control over their daily glucose fluctuations. Many patients report frustration when their HbA1c remains stubbornly elevated despite adherence to other complex regimens. How the Medication Helps: The Mechanism of Action of PrandinPrandin, with its active ingredient Repaglinide, belongs to a class of drugs known as meglitinides. Its primary function is to stimulate the pancreas to release more insulin, but crucially, it does so in a meal-dependent manner. This mechanism sets it apart from older sulfonylurea drugs. When you are considering "Prandin mechanism of action", the key concept is rapid stimulation. Repaglinide works by closing the ATP-sensitive potassium channels in the beta cells of the pancreas. This depolarization causes calcium channels to open, leading to the influx of calcium ions, which then triggers the rapid secretion of preformed insulin into the bloodstream. Because Prandin has a very short duration of action—peaking quickly and then clearing the system relatively fast—it is designed specifically to cover the glucose load introduced by a meal. This targeted approach means that Prandin is typically taken immediately before or right at the start of a meal. This timing ensures that the surge of insulin released coincides precisely with the absorption of glucose from the digestive tract. This contrasts sharply with medications that require consistent dosing hours before meals, such as some long-acting sulfonylureas like Amaryl (glimepiride). If a patient is searching for "Repaglinide rapid onset diabetes control", they are looking for exactly this characteristic. The swift action minimizes the time the body spends under hyperglycemic stress following food intake, providing a highly effective solution for those struggling with "spikey" glucose readings after eating. This targeted effect offers greater flexibility compared to some other glucose regulators. Benefits: Achieving Tighter Glycemic Control with PrandinThe primary benefit of utilizing Prandin is its exceptional efficacy in managing postprandial glucose excursions. By rapidly boosting endogenous insulin secretion precisely when it is needed most, it helps flatten those sharp glucose peaks that are often the hardest to manage with other oral agents. Clinical studies have shown that incorporating Prandin into a treatment regimen can lead to a significant reduction in post-meal glucose levels, which, in turn, contributes positively to the overall HbA1c reading. This improved control translates directly into a reduced risk of microvascular and macrovascular complications associated with chronic high sugar exposure. For individuals who monitor their glucose levels frequently, the visible improvement in post-meal readings provides immediate positive reinforcement. Another significant advantage of Prandin is its flexibility regarding meal schedules. Unlike some diabetes medications that require strict, non-negotiable timing, Repaglinide’s dosing schedule is tied directly to food intake. If a meal is skipped, the dose of Prandin should also be skipped. This adaptability is invaluable for patients whose eating patterns fluctuate or who occasionally miss a meal, offering a safety margin against inadvertent hypoglycemia—a key concern when managing insulin secretagogues. Furthermore, for patients who find injections difficult or are seeking to maximize oral therapy options before escalating to injectable insulin, Prandin offers a potent oral alternative. Many patients research "oral medication like insulin for post-meal spikes", and Prandin fits this description perfectly. This flexibility is a major selling point when compared to the rigidity sometimes required by medications like Glucotrol XL. Beyond glucose metrics, better blood sugar stability often leads to improved quality of life. Patients report feeling less lethargic after meals, experiencing fewer instances of energy crashes, and generally having more consistent energy levels throughout the day. In situations where combining multiple oral agents is necessary, such as in combination therapy, Prandin often pairs well with drugs that primarily address insulin resistance, like Metformin or thiazolidinediones. Its distinct mechanism ensures that it is not merely duplicating the effects of other drugs but adding a necessary rapid-response component to the overall treatment strategy. When exploring "Repaglinide combination therapy diabetes" options, its compatibility is a frequent positive finding. We understand that managing diabetes is a complex balancing act. That is why choosing the right tool is paramount. If you are looking for immediate, targeted control over your daily glucose fluctuations, then exploring the potential of Prandin is a vital next step in optimizing your diabetes management plan. Take the next step toward smoother glucose curves today. Consult your healthcare provider about incorporating Prandin into your regimen. General Information, Available Forms and DosagesPrandin (Repaglinide) is a prescription medication specifically indicated for the treatment of adult patients with Type 2 Diabetes Mellitus whose hyperglycemia cannot be adequately controlled by diet and exercise alone, or when the primary concern is controlling postprandial glucose levels. It is crucial to emphasize that Prandin is not intended for use in Type 1 Diabetes or for the treatment of diabetic ketoacidosis. As a rapid-acting insulin secretagogue, its utility lies in immediate glucose control rather than long-term basal regulation. When physicians evaluate "Repaglinide dosing schedule", they focus heavily on the patient's meal timing and carbohydrate intake patterns. Prandin is available in tablet form for oral administration. The standard available dosages are 0.5 mg, 1 mg, and 2 mg. The typical starting dosage for most non-insulin-treated adults is 0.5 mg taken three times daily with meals. However, dosage adjustments are highly individualized based on blood glucose response and must be made cautiously. Maximum recommended doses are generally 2 mg taken up to three times daily, ensuring the total daily dose does not exceed 8 mg. The 0.5 mg strength is often ideal for titration or for use in elderly patients or those with mild hyperglycemia concerns, allowing for precise dose escalation. For those who might be switching from older agents, understanding how Prandin compares to medications like Glyburide or Micronase (both sulfonylureas) is important, as Prandin generally has a shorter duration of action. It is essential for patients to understand the difference between starting Prandin and starting a medication like Actos (pioglitazone), which requires weeks or months to reach its full therapeutic effect on insulin sensitivity. Prandin works within minutes. Patients frequently ask about "Prandin interaction with other diabetes drugs". While it can be safely used in combination with agents like Metformin (sometimes seen as Glucovance when combined), careful monitoring is necessary to prevent hypoglycemia, especially when initiating therapy or increasing the dose. Always discuss your complete medication list with your prescribing physician. How to Use Prandin Safely and EffectivelyThe efficacy of Prandin is intrinsically linked to its administration timing. The instruction is clear: take Prandin tablets (0.5 mg, 1 mg, or 2 mg) within 15 minutes before a meal. If the patient skips a meal or eats a meal that is significantly smaller than usual (i.e., skipping a main carbohydrate-containing meal), the corresponding dose of Prandin must be skipped. This rule is non-negotiable for safety. Taking Prandin long before a meal increases the risk of hypoglycemia because the insulin surge will occur before the glucose arrives in the bloodstream. Conversely, taking it too long after the meal means the medication misses the peak glucose absorption window, rendering it less effective for postprandial control. Patients often search for "what happens if I miss a dose of Prandin", and the answer depends entirely on whether the meal is also missed. Regular self-monitoring of blood glucose (SMBG) is paramount when initiating or adjusting Prandin therapy. Blood glucose checks should ideally be performed 1 to 2 hours after the start of the meal to assess the drug's effectiveness against that specific meal. Dietary counseling remains a cornerstone of diabetes management; Prandin is an adjunct, not a replacement, for a healthy, balanced diet appropriate for diabetes. Patients should also be aware of potential cross-reactivity if they are taking medications known to affect blood glucose levels, either raising or lowering them. Patients managing Type 2 diabetes often juggle many medications, sometimes including fixed-dose combinations like Metformin + Glyburide, necessitating close communication with their endocrinologist regarding the addition of Repaglinide. Safety and Side Effects Profile of PrandinLike all anti-diabetic medications, Prandin carries potential risks and side effects that must be weighed against its benefits. The most common and serious side effect associated with Prandin, as with all insulin secretagogues, is hypoglycemia (low blood sugar). Because Prandin forces the pancreas to release insulin regardless of the current blood glucose level (though triggered by the presence of a meal), improper timing or skipping meals after dosing can lead to dangerously low sugar levels. Symptoms of hypoglycemia include dizziness, sweating, confusion, rapid heartbeat, and potentially loss of consciousness. Patients must be educated on recognizing and treating hypoglycemia immediately, typically with fast-acting carbohydrates. Other less severe but common side effects include gastrointestinal upset, such as nausea or diarrhea, and headache. Rare but important considerations include hypersensitivity reactions. Patients with known sulfa allergies should exercise caution and discuss this with their doctor, as meglitinides share some structural similarities with sulfonylureas, although the risk profile differs. Furthermore, weight gain can occasionally be a side effect, similar to what is sometimes observed with agents like Glucome (glimepiride) or older insulin secretagogues. Contraindications generally include established Type 1 Diabetes, during episodes of severe metabolic acidosis (including diabetic ketoacidosis), and in patients with severe liver impairment, as Repaglinide is primarily metabolized by the liver. Before starting any new medication, patients should thoroughly review their medical history. If you are searching for "Prandin versus sulfonylurea side effects", you will generally find that Repaglinide is associated with a slightly lower risk of prolonged hypoglycemia due to its shorter half-life, but the risk remains significant and requires diligent monitoring. Reviews and Social Proof: Real-World ExperiencesPatient testimonials frequently highlight the transformative effect Prandin has had on controlling the challenging post-meal glucose spikes that plagued them for years. Many users report that while other oral medications managed their baseline, Prandin provided the precision control needed to achieve target post-meal readings, often leading to better overall HbA1c results during follow-up appointments. One patient noted, "I used to dread eating lunch because my sugar would skyrocket to 300 mg/dL every time. Since starting Prandin exactly five minutes before eating, I now see readings closer to 180 mg/dL, which is a massive improvement." This sentiment is common among those who take the medication precisely as directed. It is also valuable to see how Prandin fits into complex regimens. Patients who were previously dependent on injectable insulin to manage mealtime spikes often report that the flexibility and convenience of Prandin—being able to swallow a pill instead of preparing an injection—significantly improved their adherence and reduced injection fatigue. When comparing experiences, patients often ask, "is Prandin better than Acarbose for post-meal control". While Acarbose (Precose) works by slowing carbohydrate digestion, Prandin actively stimulates insulin release; many users find the latter approach more effective for their specific physiology. Social proof leans heavily toward its effectiveness when timing is rigorously maintained. Of course, managing chronic conditions always involves trade-offs. Some users mention needing to be extremely vigilant about carbohydrate counting to avoid lows, especially on days when activity levels change unexpectedly. However, for the vast majority of users for whom postprandial hyperglycemia is the primary hurdle, Prandin is often cited as a highly effective, targeted therapy that brings much-needed stability back to their daily glucose profile. When looking up "Repaglinide user satisfaction rates", adherence improves significantly when patients recognize the direct, rapid feedback loop between taking the pill and their subsequent blood sugar reading. Dosage and Administration Specifics for 0.5 mg StrengthThe 0.5 mg tablet of Prandin is frequently used as the initial dose, especially for individuals who are either sensitive to medications, have lower baseline glucose excursions, or are elderly. This lower strength allows clinicians to titrate the dose upward slowly. The standard starting regimen is one 0.5 mg tablet taken three times daily (before breakfast, lunch, and dinner). If glycemic control remains inadequate after one to two weeks, the physician may increase the dosage incrementally, perhaps to 1 mg per meal, or suggest combination therapy. For example, if a patient is already taking a stable dose of a medication that works primarily on basal glucose (like Metformin), adding the 0.5 mg dose of Prandin before meals can provide the necessary mealtime boost without dramatically altering the background control. It is critical to reiterate the timing: the 0.5 mg tablet must be ingested within 15 minutes prior to eating. If the meal is small or contains very few carbohydrates, the patient should consult their doctor, as a dose reduction or omission might be warranted to mitigate hypoglycemia risk. Never adjust the dosage based on a single reading; instead, look for trends over several days. Patients who forget their dose entirely must simply wait for the next scheduled meal. They should never double up the dose to "catch up." If a patient often finds themselves researching "how to dose Prandin 0.5 mg for light meals", this indicates a need for a detailed discussion with their healthcare provider regarding portion control and personalized titration protocols. Price and Where to Buy PrandinThe cost of Prandin (Repaglinide) can vary significantly based on insurance coverage, pharmacy location, and whether you purchase the brand name or a generic equivalent. Generic Repaglinide is often more accessible and significantly more affordable than the original branded product. When patients inquire about "Prandin cost without insurance", they often find that generic alternatives are reasonably priced, making it a viable option for many budgets, particularly compared to some newer, injectable GLP-1 receptor agonists or advanced therapies like Semaglutide. To secure the best price and ensure a steady supply, it is recommended to compare prices across several local pharmacies or utilize reputable online prescription services that offer competitive pricing for generic medications. Always check if your insurance plan covers generic Repaglinide. If you have difficulty obtaining coverage or find the cost prohibitive, discussing alternatives that work similarly, such as combining sulfonylureas like Glimepiride with other glucose regulators, might be an option, although the timing flexibility of Prandin may be lost. Always purchase prescription medications from licensed and verified sources to guarantee product authenticity and quality, whether you are seeking the 0.5 mg strength or higher doses. Conclusion: A Targeted Solution for Post-Meal ControlPrandin (Repaglinide) stands out as a potent, rapid-acting oral agent specifically engineered to tackle the most common challenge in Type 2 Diabetes management: postprandial hyperglycemia. Its unique mechanism of stimulating insulin release precisely in sync with meal consumption offers unparalleled flexibility and targeted efficacy. By choosing Prandin, patients gain the power to significantly flatten dangerous blood sugar spikes, leading to better overall glycemic control, reduced long-term complication risks, and an improved sense of well-being after meals. While vigilance against hypoglycemia is necessary, the tailored dosing schedule tied to food intake provides a crucial layer of safety and convenience. If your current regimen leaves you frustrated by high numbers after eating, Prandin offers a scientifically sound and clinically proven pathway to tighter, more manageable blood sugar levels. Don't let post-meal spikes dictate your day any longer. Speak with your endocrinologist or primary care physician immediately to determine if the rapid action of Prandin is the missing piece in your comprehensive diabetes management strategy. |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Copyright © sol-anhelo.biz. All rights reserved. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||